It’s Cervical Health Awareness Month! The cervix is such an important organ–it performs many functions that help women live their lives to the fullest. Read on to learn more and for ways to keep your cervix healthy.
What is a cervix?
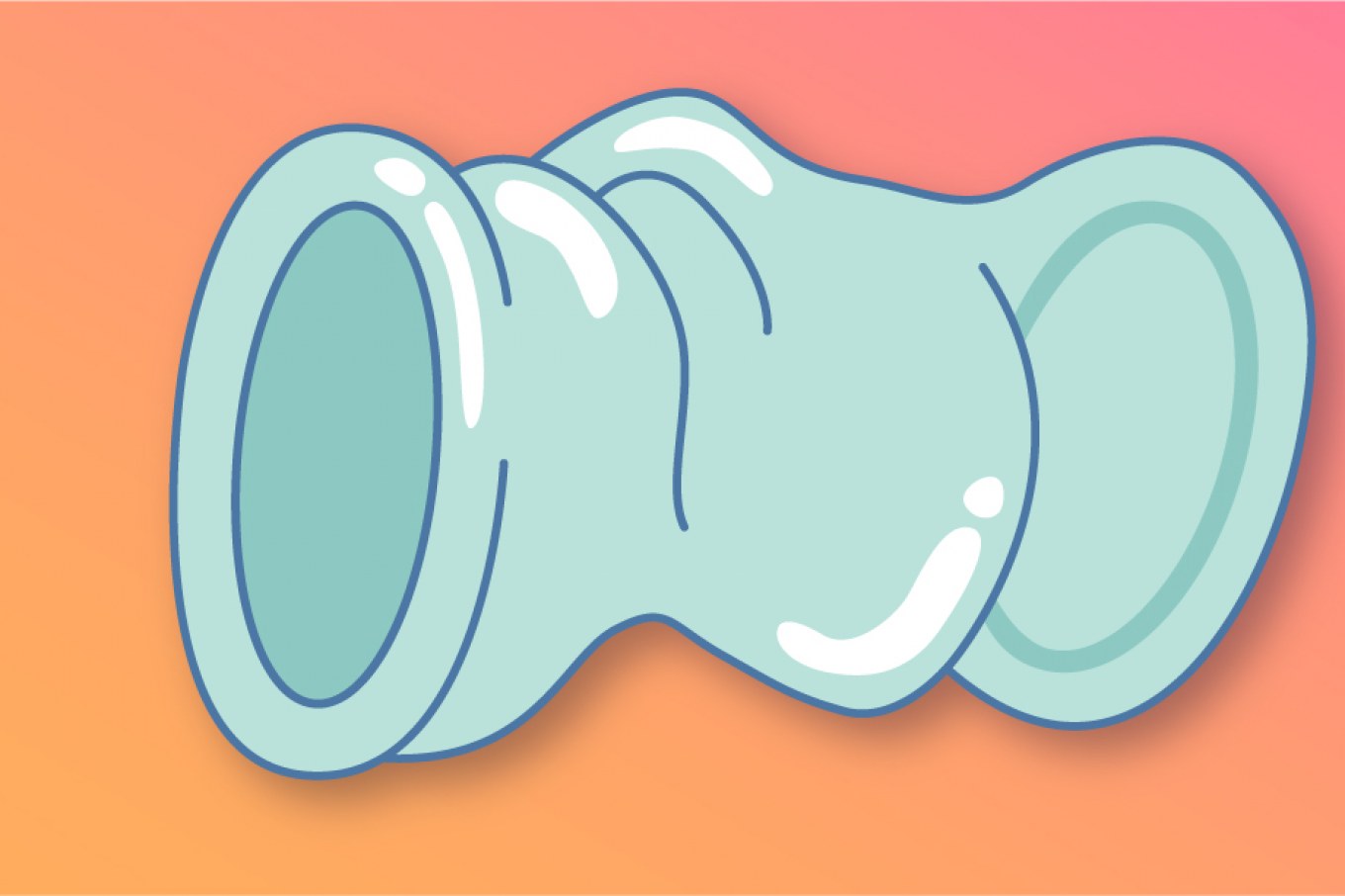
Located in the lowest and innermost part of the uterus, the cervix is a cylinder-shaped neck of tissue that connects the uterus to the vagina. The outer portion of the cervix is the called the ectocervix. It’s the part seen by doctors during pelvic exams.
There’s also the endocervix, which is a deeper portion of the cervix. And finally, the cervical os, which connects the uterus to the outer portion of the cervix. The cervical os plays an important role when it’s “that time” of the month–but more on that later.
What does the cervix do?
The cervix does a lot. From menstruation to sex to pregnancy–the cervix plays many important roles in a woman’s life. For starters, it acts as a barrier between the uterus and the vagina–so it’s one of the reasons a tampon doesn’t get lost in your body.
How else does it act during that time of the month? Well, part of the cervix, the cervical os, opens to discard blood and tissues from the uterus. And after “the flow” is done, it creates mucus to help clean the vagina and prevent infection.
For some people, the cervix is a pleasure center during deep penetrative sex. If a woman is ovulating, the cervix will change positions to increase the chance of pregnancy.
During pregnancy, the cervix creates a mucus plug that protects the fetus from infection. And during childbirth, it is the cervix that widens to allow for the passage of the baby.
Why are pap smears important?
Pap smears are important because they are the best way to screen the cervix for any signs of infection, abnormalities, or cancer. The earlier an infection or cancer is detected, the more likely it is to be treated and prevented from spreading. It also increases your chances of recovery.
What happens during a pap smear?
Pap smears are done in gynecologists offices and are relatively quick and painless. Here’s how they usually go:
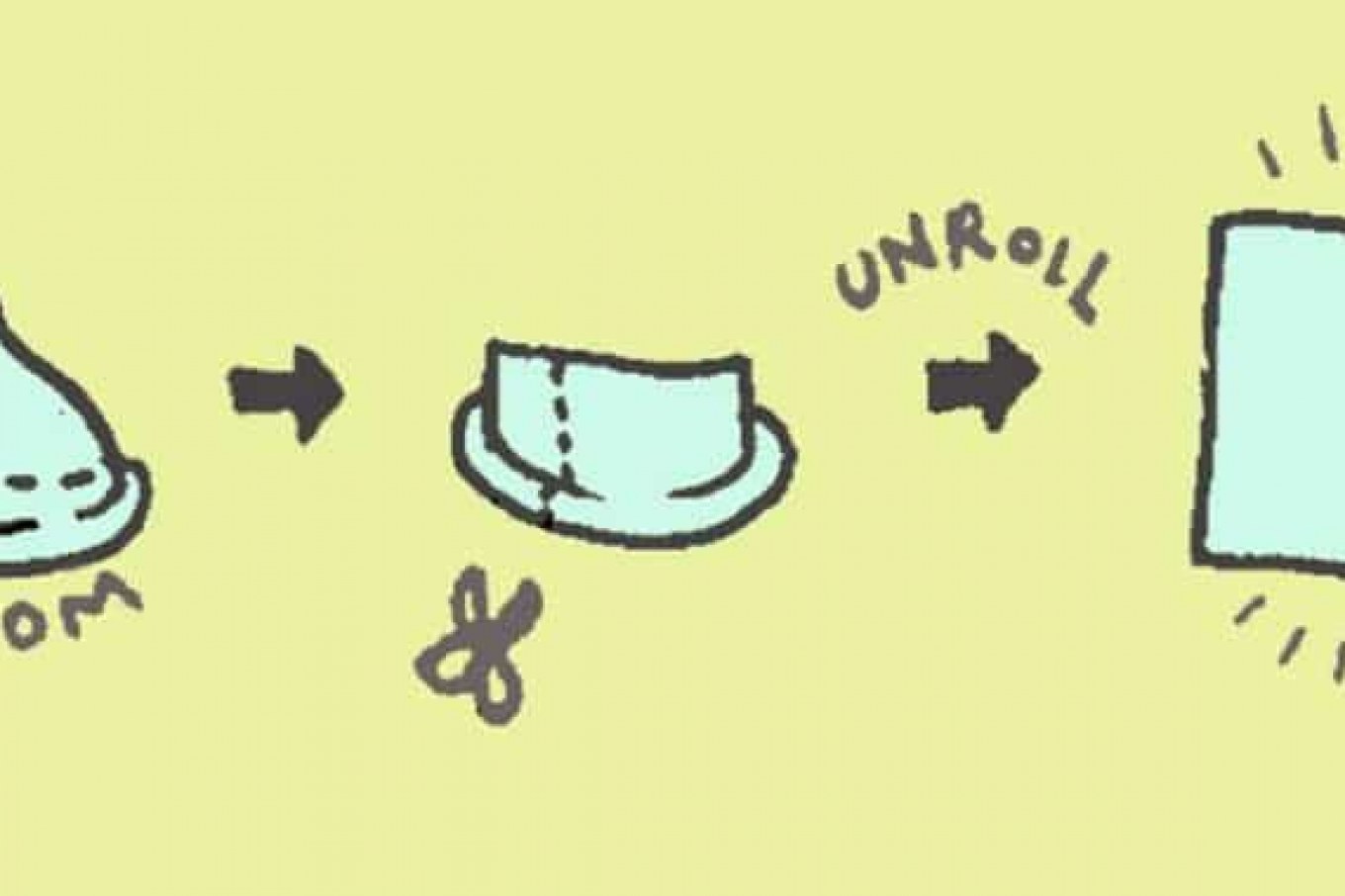
First, you will be asked to change into an examining robe and then to lie down on an exam table. Your feet will rest in stirrups and the gynecologist will begin the exam by inserting a speculum into the vagina.
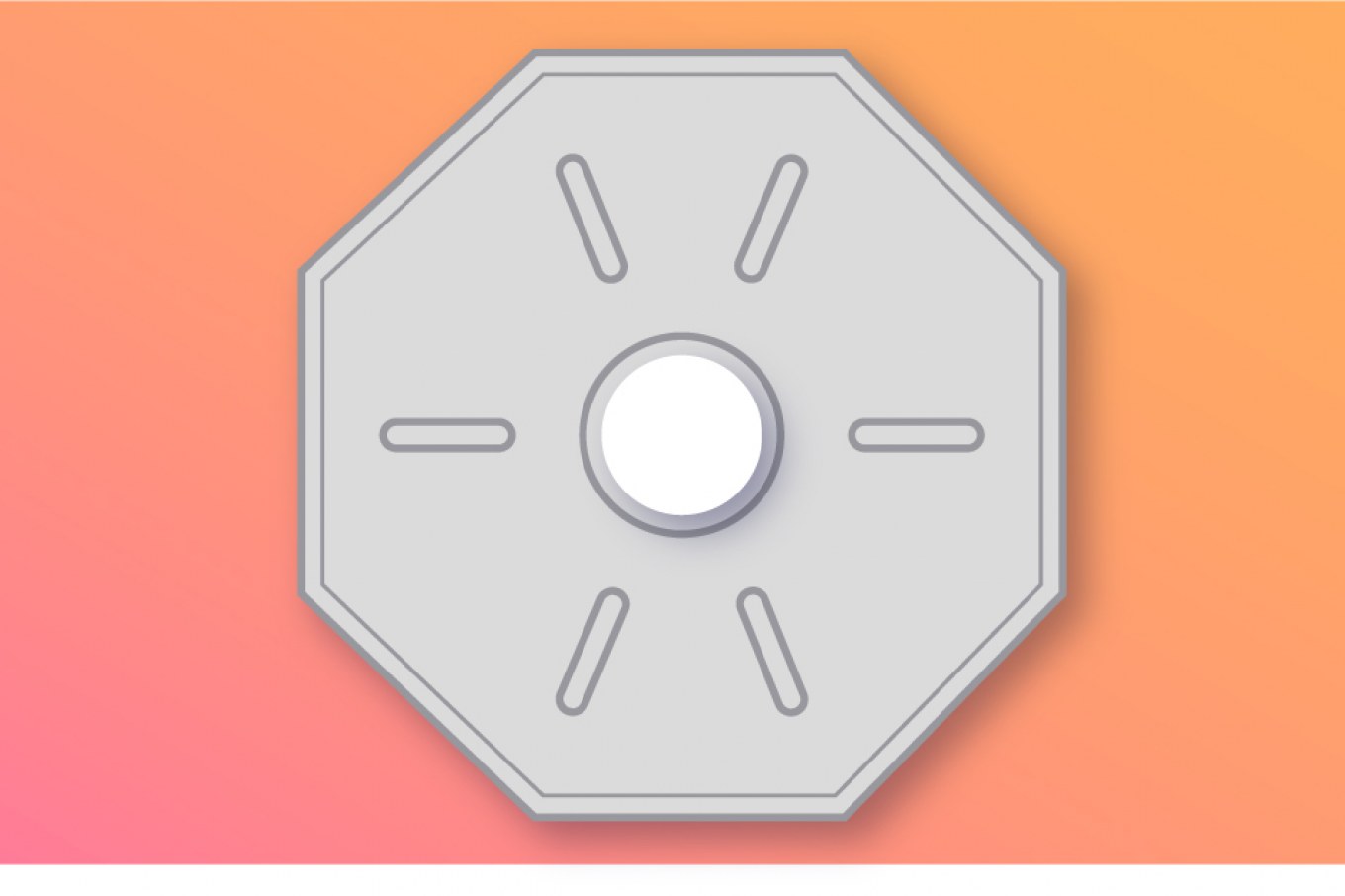
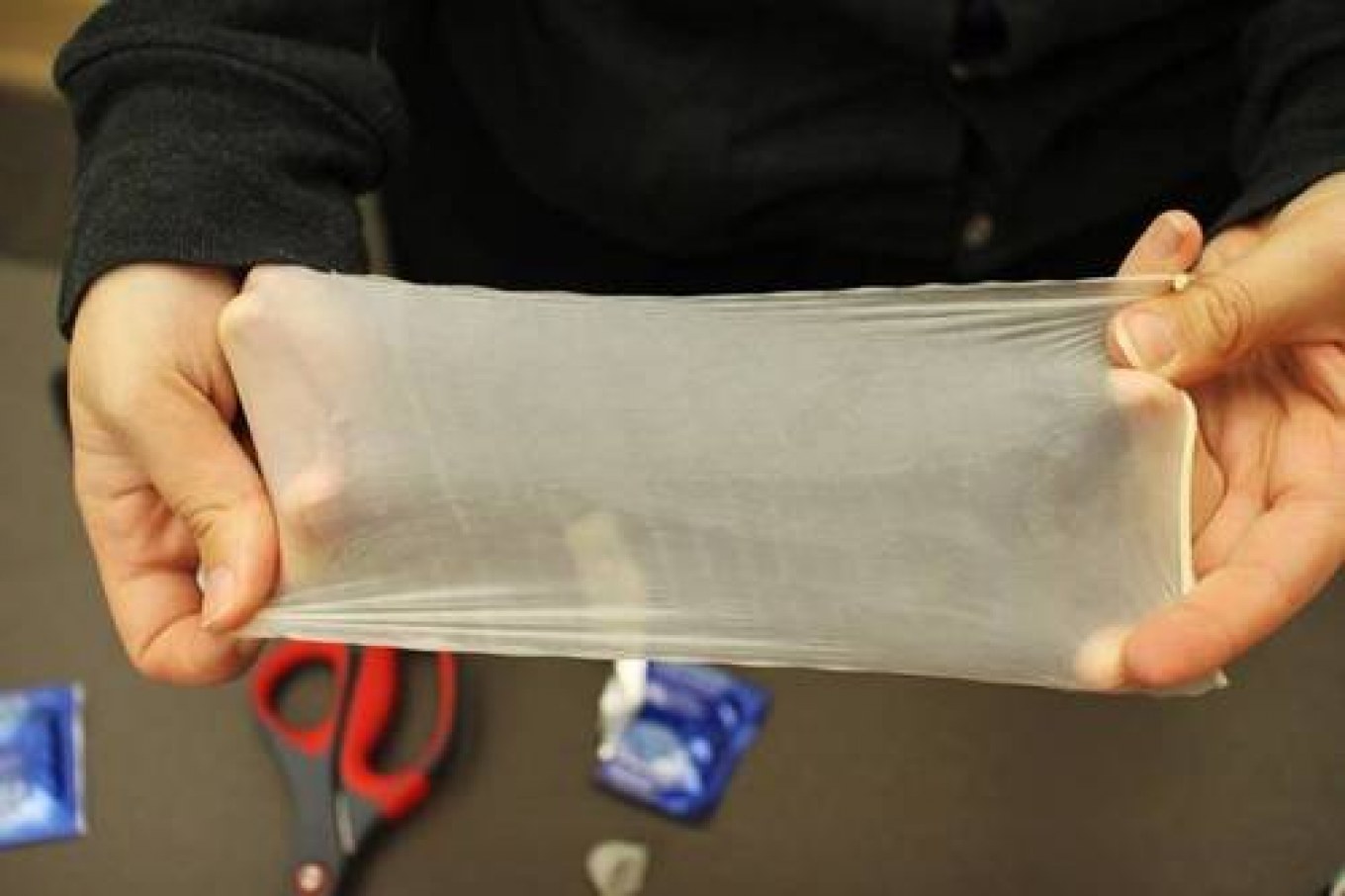
Speculums are usually made of metal or plastic and come in different sizes. They are used in pap smears to hold the walls of the vagina apart.
Gynecologists sometimes use what’s known as a Huffman speculum to examine patients who haven’t yet been sexually active to allow for a more comfortable examination. Remember: you can always ask your gynecologist for a different sized speculum if the one used to begin the exam is uncomfortable.
Once the speculum is placed, you may begin to feel pressure. This pressure shouldn’t be painful. After the speculum is secured, the gynecologist will swab the cervix with a soft brush or small spatula. After the sample is taken, the speculum is carefully removed, and the exam is over.
What are the risk factors for cervical cancer?
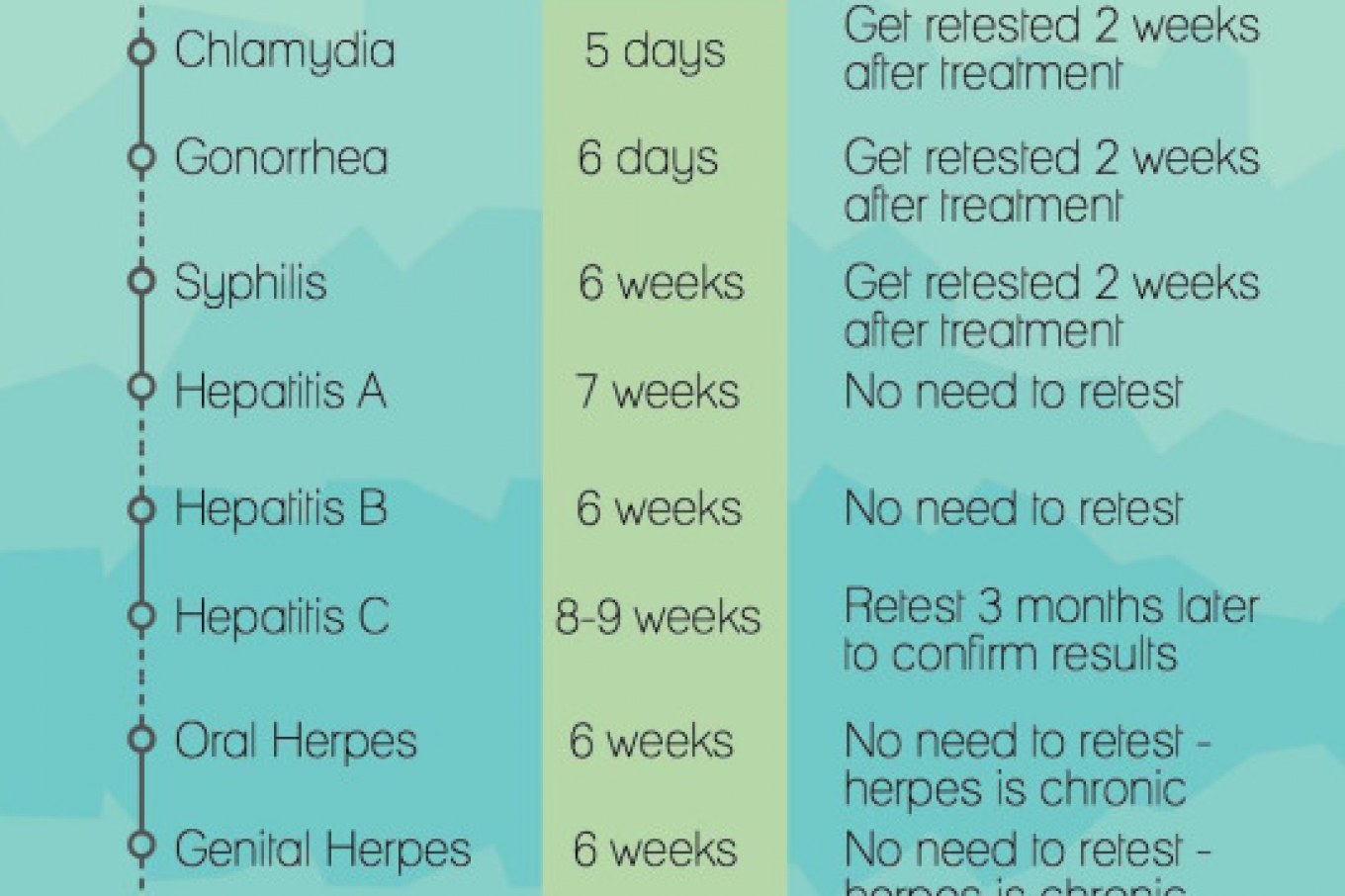
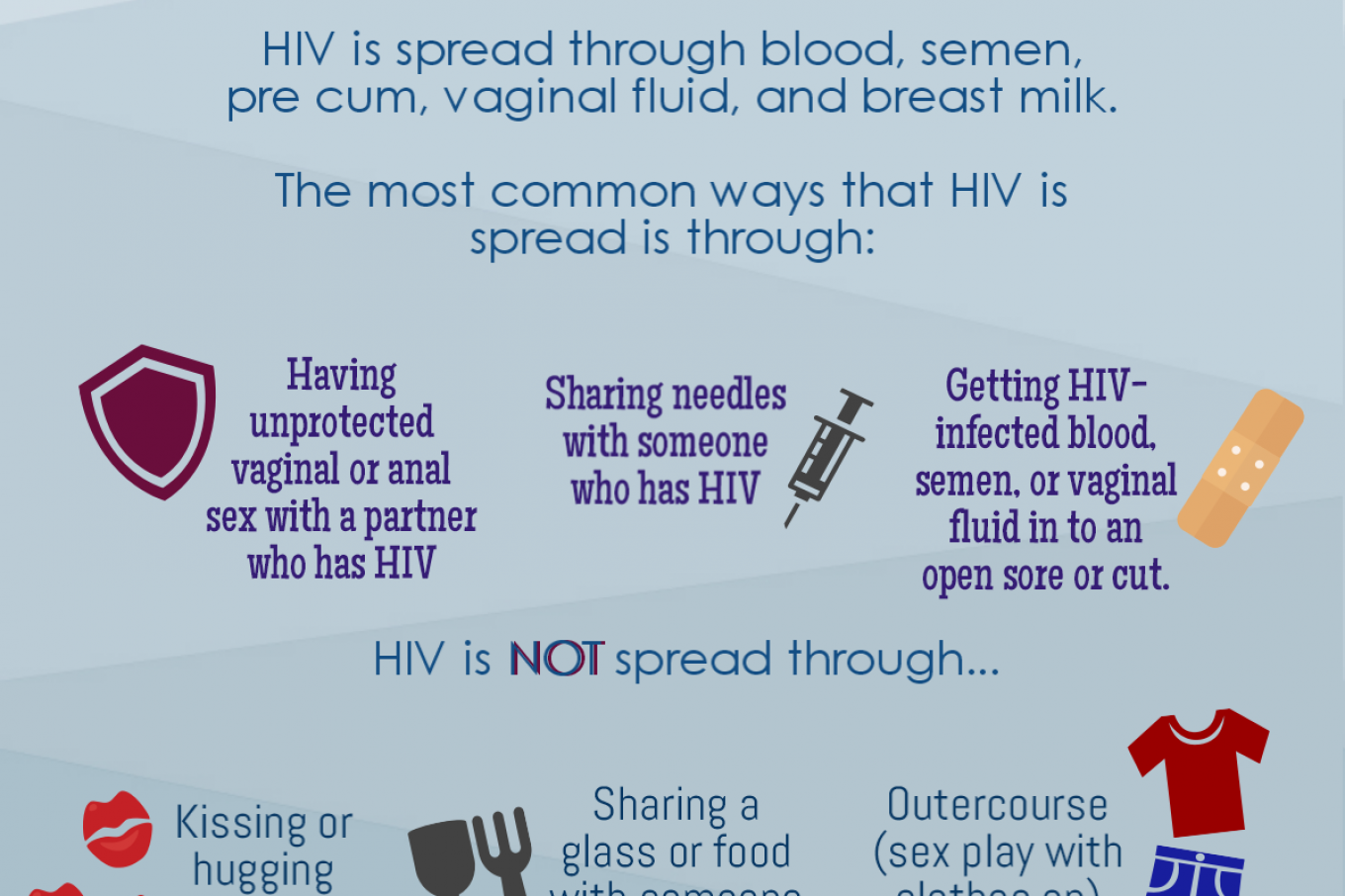
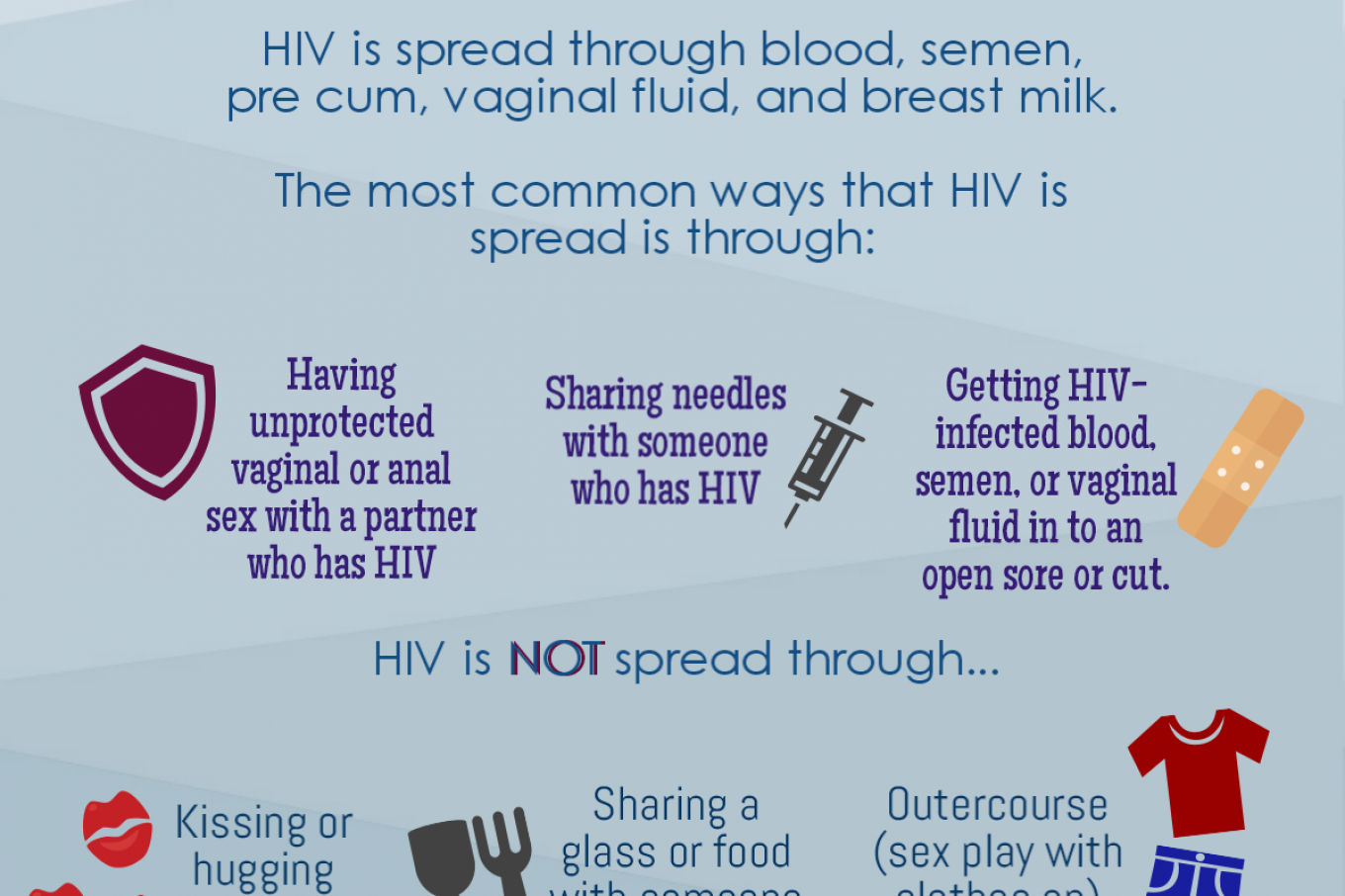
According to the CDC, almost all cervical cancers are caused by human papillomavirus (HPV). HPV is a sexually transmitted infection (STI) that has many variants (more than 40). High-risk variants of HPV may cause cervical cancer because they are not successfully controlled by the immune system.
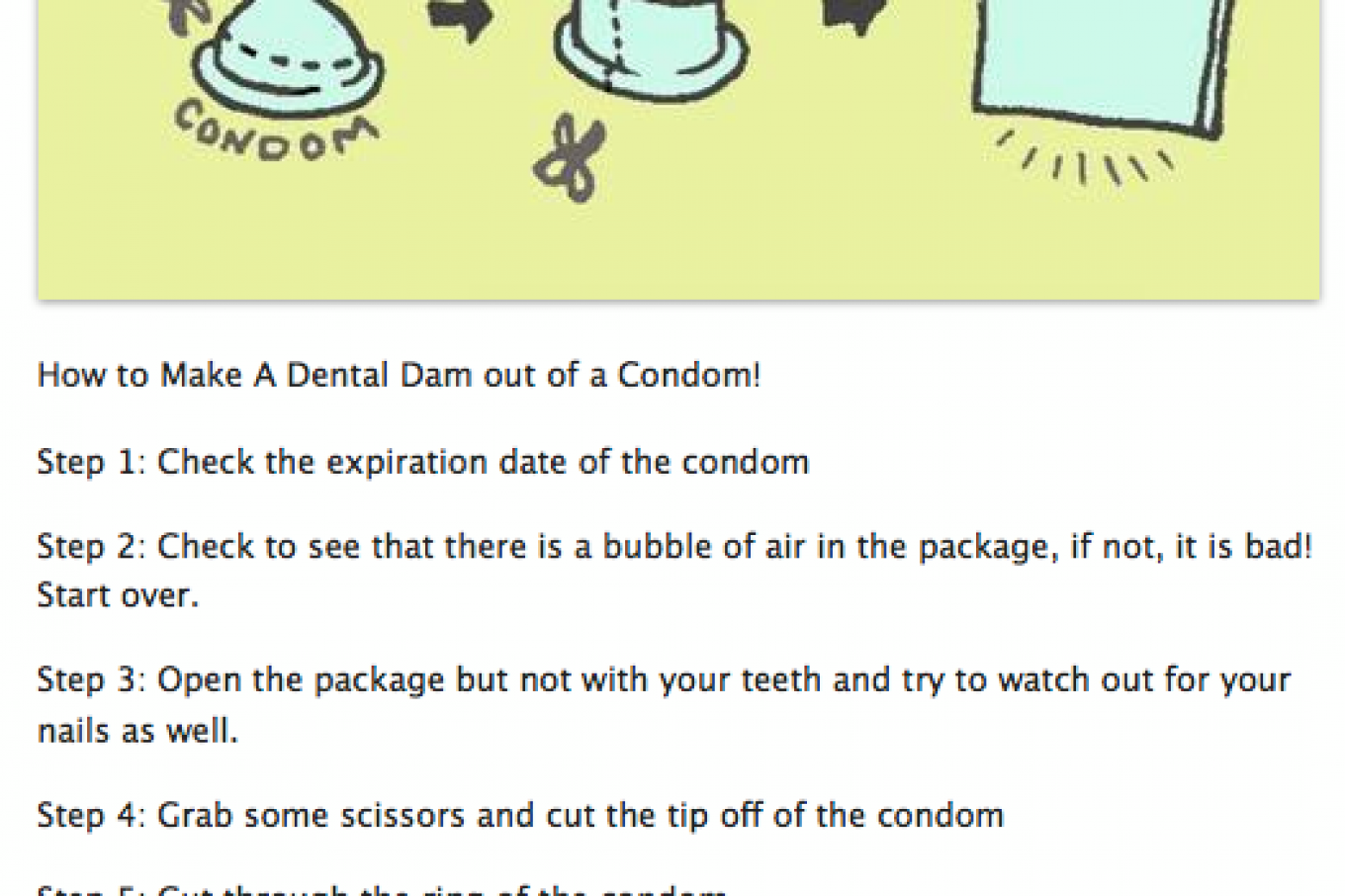
As a result, infection persists, in some cases over many years, and this can lead to cell changes in the cervix. If left untreated, these cell changes may get worse and become cancerous. Getting vaccinated with an HPV vaccine can prevent infection from variants of HPV that cause infection-related cancers or genital warts. Practicing safe sex by using condoms can also reduce your risk.
However, having HPV isn’t the only risk factor for getting cervical cancer. Smoking, having immune system deficiency, being older, or having limited access to health services all increase your risk of getting cervical cancer, according to the American Society of Clinical Oncology (ASCO).
Want to know how to keep your cervix healthy? Follow these tips:
- Get routine pap smears
- Get the HPV vaccine
- Get tested for HPV every five years
- Practice safe sex
- Look out for problematic symptoms. These may include:
- Pain during sex
- Bleeding after sex
- Abnormal discharge that may be watery, bloody, or foul-smelling
- Pelvic pain
- Boost your immunity with healthy eating and exercise
- Take time to relax and de-stress